The Neuroscience of Trauma: Understanding the Impact on Mental Health
Resilience forms the cornerstone of mental health and wellbeing. However, the architecture of our brains, having been sculpted by millions of years of evolution, is shockingly susceptible to the debilitating […]
Resilience forms the cornerstone of mental health and wellbeing. However, the architecture of our brains, having been sculpted by millions of years of evolution, is shockingly susceptible to the debilitating effects of trauma. Understanding the neurobiology of trauma provides essential insight into the working of the human brain, while providing clinicians with an informed perspective for envisioning and implementing targeted therapeutic interventions to facilitate healing.
The Neuroscience of Trauma
Trauma, typically classified as single incident or cumulative, perturbs the functional harmony of the brain and results in significant alterations in the brain’s structure and function.
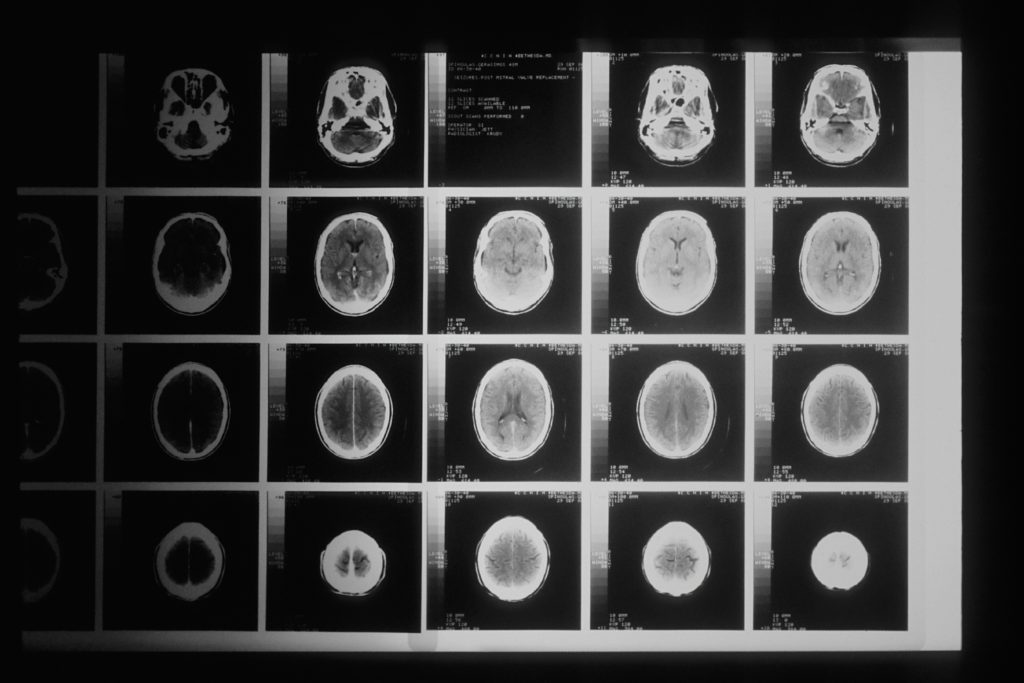
Trauma triggers the brain’s principal stress response system – the hypothalamic-pituitary-adrenal (HPA) axis, resulting in the release of cortisol that can have detrimental effects on brain structure and function if the exposure is chronic. This leads to a cascade of molecular events, impacting the hippocampus, amygdala, and prefrontal cortex, areas crucially involved in memory, emotion, and cognitive functions.
Hippocampal volume reductions have been frequently reported in victims of chronic trauma. This has significant implications on declarative and contextual memory, often manifested by intrusive recollections of the traumatic event or distressing flashbacks.
The Amygdala, implicated in fear conditioning, becomes hyperactive and hypertrophic in the aftermath of trauma. This escalated activation often results in persistently heightened states of fear and anxiety, hallmark symptoms of post-traumatic stress disorder (PTSD).
The trauma nexus of the brain also includes the prefrontal cortex which undergoes significant disruption, with signs of thinned cortex and impaired activity, affecting processes such as decision making, strategic planning, reasoning, and working memory.
Understanding the Trauma-brain Connection and Mental Health
These neurobiological alterations may give rise to a range of mental health disorders. PTSD, characterized by re-experiencing traumatic incidents, persistent avoidance of trauma reminders, negative cognition and mood, and hyperarousal, is perhaps the most commonly linked disorder with trauma.
Besides PTSD, trauma can breed other mental health conditions such as depression, anxiety disorders, dissociative disorders, and substance abuse. Moreover, there is a rising understanding that early-life trauma could also significantly contribute to the etiology of serious psychiatric conditions such as schizophrenia, bipolar disorder, and borderline personality disorder.
However, it is noteworthy that trauma does not guarantee the development of mental disorders. The outcome of traumatic events is profoundly influenced by the individual’s genetic predispositions, environmental influences, and resilience.
Implications and Actionable Steps for Clinicians
To effect meaningful change, clinicians dealing with trauma-affected individuals need to integrate this neurological understanding into their practice.
- Trauma-Informed Care: Implementing trauma-informed care approaches can help in recognizing the presence of trauma symptoms and acknowledging the role of trauma in the individual’s life and development.
- Neurofeedback: Therapies like neurofeedback, that specifically target the dysregulated neural circuits, can be beneficial.
- Cognitive Behavioural Therapies (CBT): CBT techniques can have profound effects on modulating the cognitive dysfunctions facilitated by trauma.
- Pharmacotherapy: Medications can assist in managing the biosignatures of trauma such as insomnia, anxiety, and hyperarousal.
- Promote Resilience: Encourage practices that promote resilience, like mindfulness, meditation, good sleep hygiene, regular exercise, and a balanced diet.
- Interdisciplinary Collaborations: Finally, collaborative approaches that involve interdisciplinary collaboration among neuroscientists, clinical psychologists, and psychiatrists can guide the development of comprehensive intervention strategies.
Understanding the neuroscience of trauma empowers us to unlock the shackles of trauma and provide victims a promising path towards recovery and resilience. Through trauma-informed care and evidence-based interventions that address the biological aftermath of trauma, we can guide clients in moving from surviving to thriving.
Photo by National Cancer Institute on Unsplash
Written by AI & Reviewed by Clinical Psychologist: Yoendry Torres, Psy.D.
Disclaimer: Please note that some blog posts may contain affiliate links and Sana Network will earn a commission if you purchase through those links at no additional cost to you. We use all of the products listed and recommend them because they are companies or products that I have found helpful and trustworthy. Our website is supported by our users.
